Laryngomalacia & Infant Reflux
Laryngomalacia is more common than you think
Has the pAediatrician or ent mentioned laryngomalacia?
Laryngomalacia commonly occurs in infants & very rarely into adulthood, with over half having some symptoms of laryngomalacia in the first week of life. Between 2-4 weeks, even more infants are likely to develop laryngomalacia as their airways continue to develop & symptoms. Symptoms can range from mild to severe, so each baby is going to show their own individual signs & symptoms for us to observe.
I find many parents have had the term laryngomalacia dumped on them during an appointment but nobody has taken the time to explain it, so the online searching for answer only adds to the anxieties! Parents dealing with babies experiencing breathing or feeding difficulties can be scary & stressful. No parent wants to see their child suffering.
Did they explain what it was or why it can be common in infancy?
What is laryngomalacia?
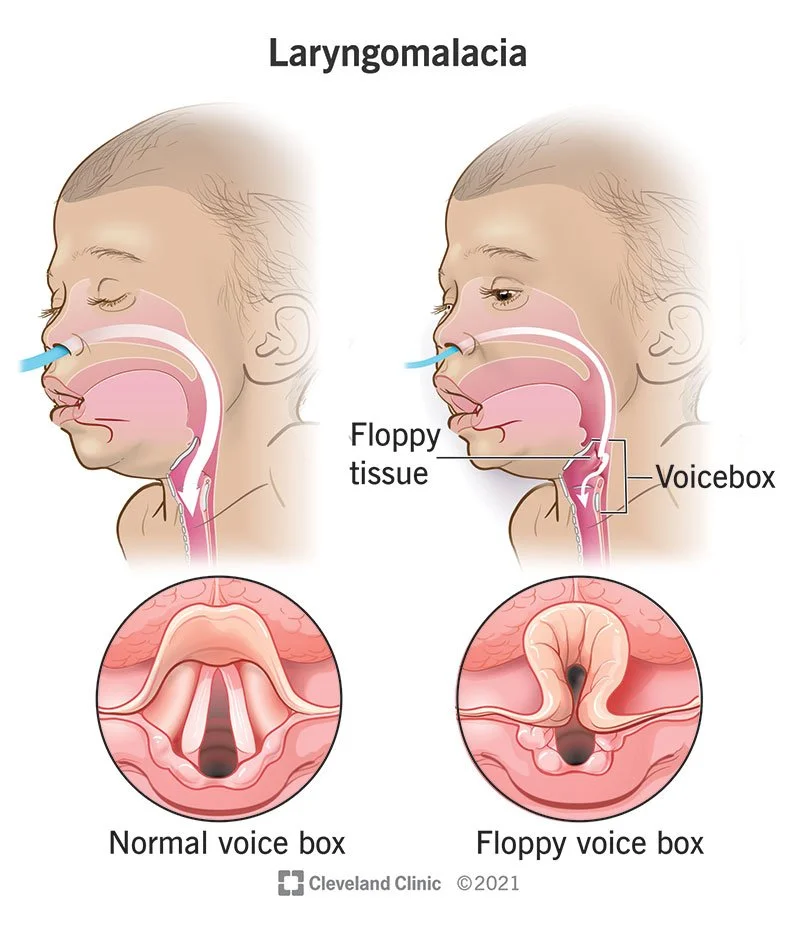
Laryngomalacia is a congenital softening of the tissues of the voice box, known as the larynx. The larynx sits just above the vocal cords & the oesophagus.
These softened tissues, namely the cartilage of the upper larynx itself, are described as 'floppy' or 'soft' & begin to impede on the airways when your baby breathes in. This causes a narrowing effect of the air pipe, which creates the high pitched, squeaky sound your hear them making.
It is the most common cause of noisy breathing in infancy, & typically improves by 12-20 months old. It is not a serious condition for most infants, but if the symptoms are more severe, like feeding or breathing difficulties & failure to gain weight/thrive, then further investigation & treatment may be necessary.
This image shows the difference anatomically between a ‘normal’ & a ‘soft’ larynx
What symptoms might you see?
With the majority of infants typically having mild symptoms of laryngomalacia, the most common symptom parents will see, or hear, is noisy breathing. This noisy breathing is usually a high-pitched, squeaky or wheezy sound when they breathe in, known as stridor.
Stridor is something that can trouble parents, because it can be worse when your baby is upset, agitated, crying or during a feed. Many babies can have mild symptoms like stridor & not have breathing or feeding difficulties that need any medical intervention. Others may have multiple symptoms that cause more worrisome signs.
Some more serious symptoms that parents may see include:
👅 Breathing difficulties, including tugging at their neck
👅 Choking or aspiration (food being drawn into the airways)
👅 Feeding issues, like difficulties swallowing, gaging or spluttering
👅 Sleep apnoea (long pauses in breathing during sleep)
👅 Restricted tongue movements or function
👅 Blue skin or blue lips (called cyanosis)
👅 Infant reflux or silent reflux
So, what's the link to infant reflux?
It is not uncommon for infants with acid reflux, or gastroesophageal reflux (GER/GERD), to also show signs of laryngomalacia too. Let's dig into why.
As parents dealing with baby reflux well know, their little one typically doesn't like to lay on their back, especially not for a long period of time. Infants that have laryngomalacia often have symptoms like reflux or silent reflux because the softened tissues haven't developed as well as they should have in the initial weeks of life. This means spit up can get up into the back of the throat, with the potential to cause discomfort.
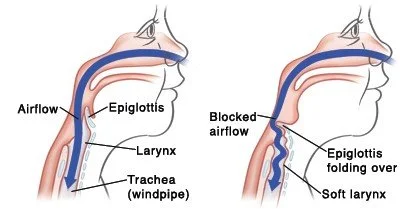
Image shows how airflow to the lungs can be blocked for an infant with laryngomalacia
This regurgitation of both milk/food & stomach acid can exacerbate symptoms when it reaches the larynx, causing further irritation & inflammation of an already compromised area. If the regurgitation is triggering coughing, spluttering, choking or breathing difficulties when your baby is on their back, it can be one of the first indicators parents see that their child is experiencing more than just reflux.
The part that (understandably) scares parents the most when it comes to reflux & laryngomalacia (whether diagnosed or not at the time) is the choking episodes & breathing issues. It is a horrible sound for a parent to hear & even more shocking to witness if they begin to choke, especially as it can happen frequently for these infants. The regurgitated material your baby brings up from the stomach into the oesophagus or mouth can get beneath the epiglottis, a small flap that protects the airways from food entering the lungs, causing aspiration. When the immature or under developed tissues of the larynx, tongue & oral cavity associated with laryngomalacia cannot perform their function properly, these symptoms can become more frequent, giving parents all kinds of stress!
Another common cause of infant reflux is aerophagia, or the excessive swallowing of air, that usually occurs during a feed. This can be the result of an oral tie or oral dysfunction during latching or feeding; in relation to laryngomalacia, a posterior tongue tie is commonly identified. If baby can't establish a deep latch with a good seal & suction motion of the tongue during feeding, air can get in & can trigger reflux afterwards. Proper function of the tongue is directly related to how the epiglottis & muscles in the larynx, pharynx & oesophagus develop & function, so it's important we establish how these tissues are interacting with one another.
When should you seek medical help?
If your baby is showing any of the signs & symptoms discussed above, it is important to find out why it is happening. Not every baby that has reflux or coughing/choking spells will have a soft larynx, but it is always advisable to seek the opinion of a medical professional if there's cause for concern.
A baby that is having frequent choking spells or aspiration, or is failing to gain weight or thrive, should, in my opinion, be seen by their pediatrician to check all is well. If concerned, contact your pediatrician to ask if visiting ER is necessary for your baby's health & wellbeing.
How I can help
If your baby has been experiencing reflux or silent reflux since birth, it is important to identify & address the root cause of it so we can reduce not only their discomfort, but also their risk of potential aspiration or choking if any food or milk is accidentally drawn into the airways.
Infants that have even mild laryngomalacia can improve drastically with the right support & guidance. I can help you identify what symptoms are associated with both the laryngomalacia & what is related to the reflux, so we can dig deeper into why your baby is experiencing these symptoms & how we can resolve them together.
If you already have a diagnosis of laryngomalacia for your little one, my Oral Function & Exercises Consultation is designed to help you understand what their oral function should be, what strategies you can implement to support your baby's development as they grow, & demonstrate oral exercises that are beneficial to their strength & development moving forward.
You do not have to do this alone
🌻🌻🌻🌻🌻
If you would like my help, you can email me, download my free reflux symptom tracker, check out my social media pages
🌻🌻🌻🌻🌻
Please note: if you are concerned about your baby's symptoms, you should seek medical advice & contact your paediatrician or a qualified provider.
This is intended for educational purposes only & does not substitute for a medical diagnosis.